For instance, a while back I had a client sending me her blood sugar charts every few days and on those charts, she always made some notes if she had questions.
Every time she sent them through, I noticed she had 3 big question marks (???) against her morning readings. And on another morning when her morning blood sugar levels were high at 160 mg/dl (or 8.9 mmol/l).
She had written:
I don't understand. 97 mg/dl (or 5.5mmol/l) last night when I went to sleep. I didn't eat anything because I didn't feel well. Humm…
Here on the DMP blog we often receive comments like:
Why is my reading in the morning higher than when I go to sleep?
My morning numbers are always high no matter what I do. When I say high I mean 190. I am so frustrated and don't understand why.
Why does my blood glucose spike in my sleep giving me a high reading in the morning when I watch all I eat at dinner time?
Do these morning situations sound familiar to you? Are you constantly questioning why you have high blood sugar in the morning?
Logically we'd think that it should be at its lowest in the morning, right?
Well don't panic, there is a reason for it, so let's explore why morning blood sugar is often higher. And then we’ll discuss what you can do to help lower blood sugar in the morning.

Why Is Blood Sugar High In The Morning?
Although it would seem logical that your body would have the lowest blood glucose level in the morning, this often isn’t the case for the following 6 reasons.
1. Glucose Happens 24/7
All the cells in the body need glucose to fuel their function, even when we sleep.
Therefore the liver can produce sugar (glucose) by breaking down body stores (glycogen), a process called glycogenolysis. The liver can also manufacture sugar (glucose) from amino acids (proteins) in a process called gluconeogenesis.
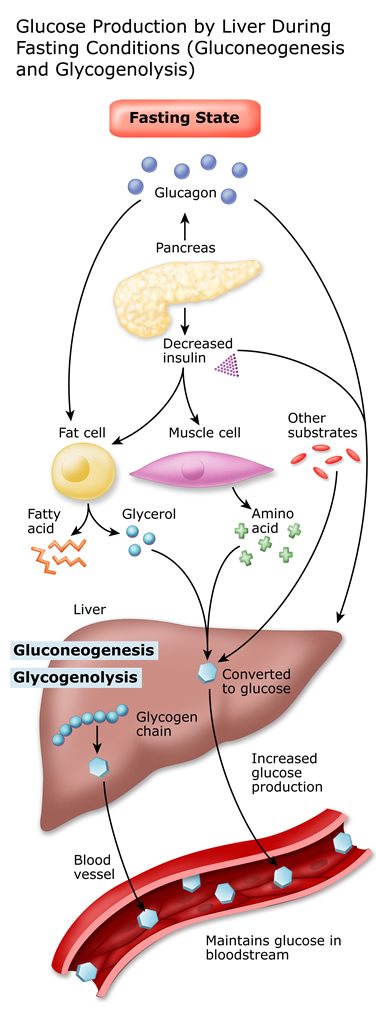
Image courtesy: University of California
These processes ensure the body and brain have adequate fuel so they can continue to go about their functions.
The point is: glucose production in the body will still occur when you don't eat or if you skip a meal because the body always maintains glucose at a certain level in order to function.
2. Hormones Raise Blood Glucose (the Dawn Phenomenon)
Around 3-4 am each morning, there are a collection of counter-regulatory hormones that are signaled in the body: glucagon, epinephrine, growth hormone, and cortisol, which result in a rise in blood sugar.
This change in hormones occurs to stimulate our awakening, to get us moving and to give us energy. This is referred to as the Dawn Phenomenon or Dawn Effect.
This is, in fact, a ‘normal' response. This occurs in everyone, diabetic or not.
However, if you have diabetes or prediabetes there is one additional factor that impacts both the overnight glucose production and the rise in glucose with cortisol, and that is decreased insulin production or decreased utilization of insulin.
3. Decreased Insulin Production or Utilization of Insulin
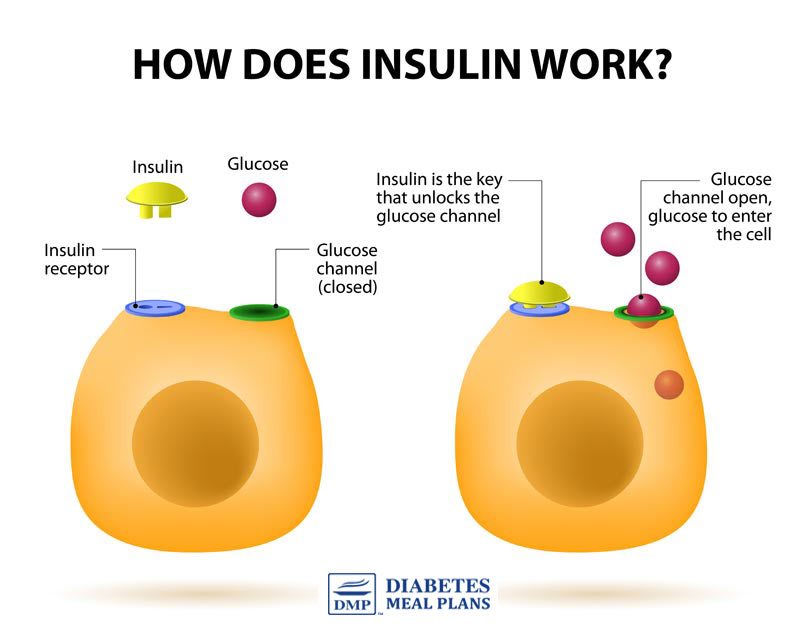
Because most people with type 2 diabetes and prediabetes have either decreased insulin levels or decreased utilization of insulin, there is either not enough insulin being produced to bring the rising blood sugar levels down, even during the night when you are sleeping.
In this scenario, your body is still producing glucose, your hormones are still doing their thing, but insulin production is low so your body is unable to counteract the effects of the glucose and hormone change.
The other scenario is that your levels of insulin resistance are preventing effective utilization of insulin, which results in high levels. You may be producing sufficient insulin, even during the night, but your cells are not opening in response to insulin, therefore glucose remains in the bloodstream.
4. Hypoglycemia is known as the Somogyi Effect
This is less common but in some people with diabetes, low blood sugar (hypoglycemia) can occur while you are sleeping.
The Somogyi effect is more common in diabetics who are insulin dependent. It's when your body's glucose levels decrease quite significantly overnight (nocturnal hypoglycemia) and as a result, your emergency system is activated. This sends messages to your hormones and organs to stimulate more glucose production to help raise your levels.
If you're insulin dependent and trying to identify why your blood sugar is so high in the morning, you might want to wake yourself up during the night to test your levels, just in case this might be your situation and your insulin dose needs to be adjusted, for instance, implementing a long-acting insulin. Or in some cases, people may choose to use a continuous insulin pump.
You can read more about the Somogyi effect here.
This is less common but in some people with diabetes, low blood sugar (hypoglycemia) can occur while you are sleeping.
The Somogyi effect is more common in diabetics who are insulin dependent. It's when your body's glucose levels decrease quite significantly overnight (nocturnal hypoglycemia) and as a result, your emergency system is activated. This sends messages to your hormones and organs to stimulate more glucose production to help raise your levels.
If you're insulin dependent and trying to identify why your blood sugar is so high in the morning, you might want to wake yourself up during the night to test your levels, just in case this might be your situation and your insulin dose needs to be adjusted, for instance, implementing a long-acting insulin. Or in some cases, people may choose to use a continuous insulin pump.
You can read more about the Somogyi effect here.
5. Poor Food Choices
Poor food choices have a profound impact on your blood glucose and A1c levels, and therefore your early morning levels too.
Regardless of the time of day, poor food choices will impact your glucose levels negatively.
Your goal is to clean up your diet and stick to eating recommended foods that support good blood sugar control.
6. Poor Overall Glucose Control
If your daily averages are coming in well above the normal healthy range for blood sugar levels, chances are your fasting levels are going to be high as well.
Good blood sugar control means keeping your blood sugar levels as close to normal as possible. And if you can keep them within the healthy range, that’s even better.
You need to know your numbers…
Aim for fasting levels:
Between 70-100 mg/dL or 4-5.6 mmol/l (optimal)
70-110 mg/dL or 4-6 mmol/l (considered good control)
70-130 mg/dL or 4-7.2 mmol/l (more liberal, but realistic for many)
2 hrs post meal the ideal is under 140 mg/dl or 7.8 mmol/l – the lower your postprandial blood glucose is post meal (for instance 120/ 6.7), the better.
There is some variation in numbers worldwide and your physician may also set you more stringent goals, or more lenient goals.
The point is: keep an eye on your numbers. If you've constantly got numbers that are running high during the day, chances are they are going to be even higher in the mornings.
Your goal is to bring your blood sugar levels within a healthy range, then naturally the morning levels do come down as well.
Still, even when you have good control of your daily levels, those morning numbers may still be a little high.
So what can you do? Let’s look at some proven strategies.
Lifestyle Strategies To Lower Morning Blood Sugar Levels
The truth is, that despite the fact we know the Dawn Phenomenon exists and worsens morning blood sugar in those with diabetes and prediabetes, researchers still haven’t solved exactly how to lower morning levels.
However, try some of the following methods to see if they work for you. Every person is different and while there is no one proven method for lowering morning levels, many people do report one, or a combination of the following helps.
Apple Cider Vinegar & Cheese Before Bed
One small study found that having 2 tablespoons of apple cider vinegar with 1 oz (28 g) cheese (which is just 1 slice cheese) before bed may help reduce morning glucose by 4% to 6%.
Cheese on its own may reduce it by 2% but the acetic acid in the vinegar exerts additional positive influence. The best apple cider vinegar to use is this one by Braggs.
Have a Bedtime Snack
The best type of snack is a protein/fat snack combined, not something high in carbs.
Here are a few ideas:
A tablespoon of natural peanut butter (great on pieces of celery for some fiber filling goodness)
A small piece of chicken with avocado or 5 olives
A small handful of macadamia nuts
A couple of slices of cheese
Sleep Soundly
Make sure you get a good restful sleep every day because lack of sleep can increase cortisol production (your key stress hormone) and this pushes glucose levels higher. Sleep quality has a big influence on blood sugar levels.
Avoid Alcohol
Although drinking alcohol might seem relaxing it is best to steer clear of it because it’s actually a stimulant and prevents deep REM sleep.
Eat Protein In The Morning
To help bring blood sugar levels down, eat something when you get up but make sure it’s a protein – or a balanced protein/fat/veggie breakfast such as a mixed veggie egg scramble.
If you go and eat loads of carbs for breakfast when your blood glucose is already high, it will only push it up further. The message here is: toast and cereals are often the worst offenders.
Eat Well Every Day
Morning blood sugar levels are all tied up with everything else you do throughout the day.
And one of the best ways to manage your diabetes or prediabetes is to eat a healthy diet every day – eat the right type of carbs, eat the right amount of carbs, and minimize the most problematic foods – the high carb offenders: sugar, bread, rice, pasta, cereals, and potatoes.
The food you eat has a direct impact on your blood sugar and A1c levels. And the more controlled you can keep your blood sugars overall, the better your morning sugars will be as well.
You'll find plenty of diet resources on our website. And if you need further help, consider joining as a member.
Supplements to Help Lower Morning Blood Sugar Levels
A variety of supplements have been shown to be effective in reducing fasting glucose levels.
Cinnamon
The average results from two months of cinnamon supplementation at about 3g/day is a reduction in fasting blood glucose by 11.8 mg/dl (0.66 mmol/l).
Polyphenols in cinnamon provide many benefits such as enhancing insulin signaling, improving glucose transport into cells, and reducing insulin resistance.
Chromium
A review of chromium supplementation found that fasting blood glucose can be reduced by 9 mg/dl (0.5 mmol/l) to 31 (1.72 mmol/l).
Researchers suggest this is due to enhancement of insulin action.
Garlic
Taking approximately 300 mg of garlic powder for 8-24 weeks has been shown to reduce fasting blood glucose by approximately 35.8 mg/dl (2 mmol/l).
Researchers suggest garlic helps enhance insulin sensitivity, exerts insulin-like activity, enhances pancreatic beta cell function and inhibits carbohydrate metabolism.
L-Carnosine
L-carnosine 1000 mg per day for 12 weeks showed a 13.1 mg/dL (0.7 mmol/l) reduction in fasting blood glucose levels.
L-carnosine is naturally found in muscle tissue and when taken as a supplement helps modify glucose metabolism, provides antioxidant, protects against glycation and reduces inflammation.
Aloe Vera
A review of aloe vera found a reduction in fasting glucose levels by 46.6 mg/dL (2.6 mmol/l). Aloe vera was either taken by supplement 50-300 mg per day, or juice 15 – 30 mL.
Although the exact mechanisms are unclear, proposed mechanisms include the expression of the genes related to glucose metabolism and reduced insulin resistance. Aloe vera contains over 75 active components, some of which are trace elements of chromium, magnesium, manganese, and zinc that are important in the metabolism of glucose.
Berberine
The effects of berberine on fasting blood sugar levels is very impressive. When people with type 2 diabetes were given 500 mg of berberine per day, 3 times per day, for 13 weeks, fasting blood glucose reduced by 68 mg/dL (3.78 mmol/l).
Berberine has many potent glucose-lowering properties. If you’d like to learn more about it, we’ve written about berberine extensively over here.
Many of the above supplements have also been shown to control blood sugar overall, along with lowering A1c, as well as providing several other benefits.
The best rule of thumb here is not to go out and take every single supplement, but try taking one supplement for a time and see if it exerts any benefits for you. If not you can try exchanging it for another one to evaluate its effects.
Always be aware that any blood sugar lowering supplements can potentially cause low blood sugar (hypoglycemia). You should always seek medical advice before supplementing, especially if taking medications.
Please pin, tweet or share; then keep on reading – thanks!

Unfortunately there is no one size fits all solution to solve the high blood sugar in the morning dilemma. Sometimes people can do everything possible and still have morning levels that always come in a little high.
Hopefully in the near future, researchers will uncover a way we can solve the issue more permanently. But in the meantime, the best thing you can do is bring your daily levels down within a healthy range and maintain them there, as this will also influence morning levels.
Second to that you can try some of the strategies above to see if they make a difference for you.
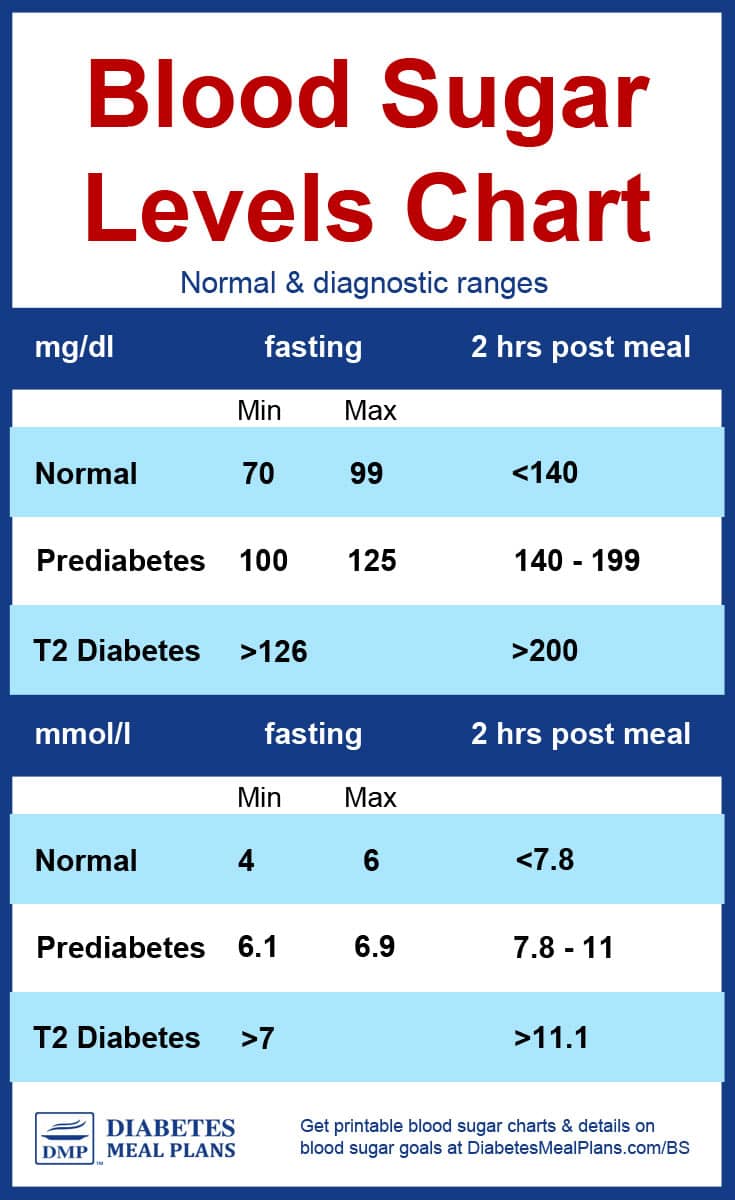
Diabetes Blood Sugar Levels Chart
Normal Blood Sugar Levels
Fasting glucose – 70-99 mg/dl or 4-6 mmol/l (Note: there is some debate about the normal range in mmol/l, ranging from 5.5 to 6 mmol/l)
2 hours post meal glucose – Less than 140 mg/dl or less than 7.8 mmol/l
Pre-diabetes – also called impaired fasting glucose or impaired glucose tolerance
Fasting glucose – 100-125 mg/dl or 6.1-6.9 mmol/l
2 hours post meal glucose level – 140-199 mg/ dl or 7.8-11 mmol/l
Diabetes
Fasting glucose – More than 126 mg/dl or more than 7.0 mmol/l
2 hours glucose level – More than 200 mg/dl or more than 11.1 mmol/l
Fasting glucose – 70-99 mg/dl or 4-6 mmol/l (Note: there is some debate about the normal range in mmol/l, ranging from 5.5 to 6 mmol/l)
2 hours post meal glucose – Less than 140 mg/dl or less than 7.8 mmol/l
Pre-diabetes – also called impaired fasting glucose or impaired glucose tolerance
Fasting glucose – 100-125 mg/dl or 6.1-6.9 mmol/l
2 hours post meal glucose level – 140-199 mg/ dl or 7.8-11 mmol/l
Diabetes
Fasting glucose – More than 126 mg/dl or more than 7.0 mmol/l
2 hours glucose level – More than 200 mg/dl or more than 11.1 mmol/l
Blood Sugar Levels Chart
The above chart and the one below are exactly the same, in different formats.
Category Fasting value Post prandial / aka post meal
Minimum Maximum 2 hours after meal
Normal 70 mg/dl 99 mg/dl Less than 140 mg/dl
4 mmol/l 6 mmol/l Less than 7.8 mmol/l
Pre-diabetes 100 mg/dl 125 mg/dl 140-199 mg/dl
6.1 mmol/l 6.9 mmol/l 7.8-11 mmol/l
Diabetes More than 126 mg/dl More than 200
More than 7 mmol/l More than 11.1 mmol/l
These are the diagnostic ranges. As you can see, the “normal” range for fasting glucose is under 100 mg/dl or 6 mmol/l. Though just to note, there is some debate about the normal range in mmol/l, ranging from 5.5 to 6 mmol/l. So depending what chart you look at, you may see either of those numbers.
After a meal, the maximum reading you ideally want to see is 140 or 7.8.
If you're getting readings above this, you would be diagnosed with prediabetes or type 2 diabetes, as shown in the charts above.
Diabetes Blood Sugar Level Goals
Upon waking before breakfast (Fasting)
70-130 (Ideal under 110) mg/dl
4-7.2 (Ideal under under 6.1) mmol/l
Two hours after meals
Under 180 (Ideal is under 140) mg/dl
Under 10 (Ideal is under 7.8) mmol/l
Bedtime
90-150 mg/dl
5-8.3 mmol/l
The above levels, for people diagnosed with type 2 diabetes, are the general goals set by the American Diabetes Association and the American Association of Clinical Endocrinologists.
As suggested earlier, there is some variation in the blood sugar levels goals set by different organizations. And additionally, your physician or healthcare team may set your goals at a more stringent level.
For instance, fasting levels:
Between 70-100 mg/dL or 4-5.6 mmol/l (optimal)
70-110 mg/dL or 4-6 mmol/l (still good control)
70-130 mg/dL or 4-7.2 mmol/l (more liberal, but realistic for many)
Once you have a type 2 diabetes diagnosis, the overall goals you should aim for is to get your blood sugar levels as close to “normal” “optimal” levels as you possibly can.
BUT, as suggested above, often goals are set with higher targets initially. For instance, if you have a high reading of 250 or 300 (13 or 17), your physician or health practitioner may recommend 200 (11.1) be an initial goal, then 180 (10), before gradually working toward 140 (7.8) and lower.
The reason this is often recommended is you can experience symptoms of hypoglycemia(low blood sugar) if you bring your levels down very quickly. So working toward tighter and tighter control does take some time.
You should work with your healthcare team on this. But overall the most optimal targets to work toward are a fasting glucose under 100 mg/dl or 6 mmol/l. And an after-meal reading below 140 or 7.8.
The Visual Version
Please pin, tweet or share this chart to help others – thanks!
Commonly Asked Questions About Blood Sugar Levels
What is the difference between blood sugar and A1c?
Blood sugar is a daily reading while A1c is a blood test that measures your average blood sugar from the previous 3 month period.
Will weight loss help with my diabetes management?
Yes, by default weight loss helps because it reduces inflammation in your body and improves overall metabolic function. However, weight loss alone won't lower blood sugar levels. You often have to make several diet and lifestyle changes to bring your levels within normal range.
I've been prescribed Metformin, will that help with my blood glucose levels?
Yes, Metformin is one of the most commonly prescribed diabetes medications worldwide. It belongs to a class of medications known as “Biguanides,” which lower blood glucose by decreasing the amount of sugar put out by the liver. And it is one of the medications that does not increase weight gain.
Why does high blood sugar cause complications like neuropathy?
The body is designed to have a blood sugar level within a certain range, with a maximum of 140 (7.8) after meals. Levels above normal for extended periods promote inflammation in the blood vessels throughout the body, along with damage to cells – simply because the body isn't designed to operate with levels above normal.
Diabetic neuropathy is damage to the nerve vessels resulting from chronically high blood sugar – meaning long-term, not a few high readings now and then. Other types of diabetes complications (nephropathy, retinopathy, etc) are also caused by the same factors.
What type of diet helps to lower blood sugar levels?
Scientific research indicates that a low carb diet is a great dietary pattern for improving blood sugar, A1c, weight, cholesterol, and other factors.
Carbohydrates are the main nutrient that influences your blood sugar levels. The type is important, but the amount has the greatest impact on both daily blood glucose and A1c measurements.
Is there a different blood sugar levels chart by age?
No. The human body was designed to have blood sugar levels within a ‘normal' range, regardless of your age.
However, different blood sugar level goals are set for each individual person, particularly children and the elderly.
The diabetes organization in my country lists different levels, why are these different?
It can make it confusing when different organizations list different values. And unfortunately, there is no one recognized value at this point, although there should be.
Here are the organization listings for some parts of the globe:
American Diabetes Association
List the normal range between 70-99 mg/dl (3.9-5.6 mmol/l).
They suggest blood glucose goals for people with type 2 diabetes are:
80-130 mg/dl before meals (4.4-7.2 mg/dl)
Less than 180 mg/dl after meals (10 mmol/l)
Diabetes Australia
List the normal range between 4.0-7.8mmol/l.
They suggest blood glucose goals for people with type 2 diabetes are:
6-8 mmol/l before meals (108-144 mg/dl)
6-10 mmol after meals / 108-180 mg/dl
Diabetes UK
List the normal range between 4-6 mmol/l (72-108 mg/dl) when fasting. And up to 7.8 mmol/l (140 mg/dl) 2 hours after eating.
They suggest blood glucose goals for people with type 2 diabetes are:
4-7 mmol/l before meals (72-126 mg/dl)
Under 8.5 mmol/l after meals (153 mg/dl)
Diabetes Canada
Like Diabetes UK, they suggest blood glucose goals for people with type 2 diabetes are 4-7 mmol/l before meals (72-126 mg/dl).
5-10 mmol/l after meals (90-180 mg/dl), or if A1c goals are not being met, it should be reduced to 5-8 mmol/l (90-144 mg/dl).
Hopefully, we will see organizations worldwide list the same glucose readings in future so there is not such a confusion.
Can these charts be used as a pre-diabetes blood sugar levels chart?
Yes. The charts contain the numbers for prediabetes as well. And you can use the charts to track your food intake and daily numbers, along with exercise or other notes you want to include.
Is daily blood glucose monitoring recommended?
If you have type 2 diabetes or prediabetes, daily self-monitoring using a blood glucose meter(which involves a simple finger-prick test), can be a great way to understand what is happening in your body so you can bring your levels under control.
How often should I take a blood sugar sample?
There is wide variability on how often to monitor, depending on the state of your diabetes and treatment. But, most people monitor 1-2 times daily – fasting (first thing in the morning) and 2 hours after the biggest meal. For your after-meal (postprandial) blood sample, time from your first bite of food.
If you’re newly diagnosed or trying to gain better control, it can be helpful to monitor more frequently so you can assess your progress and work on changing diet and lifestyle habits to support your goals.
One thing that is helpful with mealtimes is “monitoring in pairs.” To monitor in pairs you check your levels before, then 2 hours after a meal. It’s a great way to get an indication of the effect of foods and the number of carbs you’re consuming. If you log your numbers and your daily food intake and lifestyle habits, you will soon see patterns emerging and then you can make the necessary adjustments to your dietary routine.
When you download our free blood sugar chart below, we'll also provide some blood sugar logs so you can record your blood sugar readings.
Well, there you have it. Hope you find this information helpful and if you do please pin it and share it around to help others. Thanks!
Please pin, tweet or share this info to help others – thanks!
Source: http://diabetesmealplans.com/
No comments:
Post a Comment